
Guest post by Youssef Soliman, medical student at Assiut University and biostatistician
Clinical trials are the mainstay of medical innovation, but they are also notoriously expensive and resource-intensive. Funding for clinical trials comes from a wide variety of sources, yet the vast majority of funding typically comes from pharmaceutical sponsors who have the greatest stake in a trial’s success [1]. This reliance on industry funding, coupled with the immense costs of conducting trials, makes securing and managing financial support one of the top challenges in clinical research.
Inefficient financial planning or funding shortfalls can derail promising studies, delay life-saving treatments, and even introduce bias into scientific outcomes. In this article, we examine the major challenges in clinical trial funding and outline best practices to overcome these hurdles, ensuring trials are financially sustainable, ethically sound, and positioned for success.

Clinical trials often require multimillion-dollar budgets, spanning multiple phases over many years. Bringing a new drug to market is estimated to cost around $985 million on average, with clinical trial expenses accounting for a substantial portion of that figure [2]. These high costs stem from extensive personnel needs, site operations, data management, regulatory compliance, and patient care. Trials frequently underestimate timelines and expenses, leading to cost overruns or funding exhaustion before completion [2].
Every delay, whether due to slower patient enrollment, protocol amendments, or unexpected complications, translates into added expenses. It’s no surprise that funding was by far the most cited challenge faced by organizations running clinical trials. As one industry survey highlighted, trial costs can quickly balloon with each additional participant, study site, or specialized test, and broader economic conditions can tighten the flow of capital for research [3]. Thus, managing the high cost of trials and doing so efficiently remains a fundamental challenge.
Create a trial budget with AI
While pharma and biotech companies finance many trials, investigators in academia or non-profit sectors often compete for scarce grant funding from government agencies and foundations. Public funding (e.g. NIH grants) is limited and highly competitive, and even industry sponsors prioritize projects likely to yield profitable results. A meta-study of 200 trials found that 58% were government-funded and 40% funded by private companies, with only about a quarter receiving support from non-profit organizations [1].
This illustrates how much trial research leans on governmental and industry sponsors. Smaller or early-stage studies, such as investigator-initiated trials or those targeting rare diseases, can struggle to attract sponsors in a crowded field of compelling research needs. Start-ups and pre-commercial biotech firms may find their clinical programs delayed if investors pull back amid economic uncertainty. Even for funded trials, there may be funding caps or stipulations that constrain budgets for salaries or specific activities, requiring investigators to do more with less. In short, the funding pie is finite, and many worthy trials vie for slices of it. This competition means researchers must not only design sound studies but also craft compelling financial proposals to convince funders their trial is worth the investment.
Heavy reliance on a single industry sponsor can introduce implicit biases, intentionally or not, in trial design, data interpretation, and reporting. For instance, one analysis of thousands of trials found that studies primarily funded by pharmaceutical companies were significantly more likely to report favorable outcomes (risk ratio ~1.27 for positive efficacy results) compared to those with other funding [1].
This doesn’t necessarily imply methodological fraud; often it reflects systemic biases, such as only pursuing trials on drug candidates likely to succeed or selectively publishing positive findings. Additionally, the lack of transparency in funding sources can be problematic. In the Hakoum et al. survey, many trials nominally backed by non-profit groups were in fact indirectly funded by corporations, and about half of those ties went unreported in publications [4].
Inadequate disclosure of who is paying for a trial and what role funders play (study design, data analysis, authorship, etc.) can undermine trust in the findings. Only about half of the trials in that study clearly described the role of their funders. Conflict of interest concerns are real. Without proper oversight, funders might influence protocols or data reporting, consciously or otherwise. All of this underscores a key challenge: Ensuring funding arrangements do not compromise scientific integrity. Trials must maintain transparency and independent governance so that outcomes are driven by patient data and science, not by financial agendas.
Ensuring adequate funding throughout a clinical trial’s lifecycle requires proactive planning, diversification, and rigorous oversight. Below are key best practices that trial sponsors and researchers should adopt to navigate funding challenges:
Start with a realistic, detailed budget that captures all projected costs of the trial. This includes obvious direct costs (staff salaries, patient visits, laboratory tests, investigational product manufacturing, data management systems) and often overlooked expenses like IRB fees, long-term data storage, insurance, and patient travel reimbursements. Engage both scientific and financial teams in this planning. Critically, identify hidden costs early.
For example, expenses from serious adverse events (SAEs) that may require additional treatment or monitoring, costs of potential protocol amendments (re-consenting patients, updating documents, retraining staff), and extra site monitoring visits if a site underperforms [5]. By accounting for these contingencies upfront, you reduce the risk of budget surprises mid-trial. Studies often fail financially because planners assumed an ideal scenario; instead, plan for the messy reality of clinical research.
Given the unpredictability of trials, it’s prudent to set aside contingency funds as a buffer for unforeseen events.
Every trial can face setbacks like slower enrollment than expected, a key site dropping out, equipment breakdowns, or new regulatory requirements. Allocate extra funds so that such surprises do not halt the study. The contingency should be proportionate, enough to cover a few significant disruptions without excessively inflating the budget. This financial cushion provides peace of mind to sponsors and investigators that the trial can weather reasonable hurdles without going back to funders for emergency money. It’s far easier to justify a slightly larger initial budget with built-in flexibility than to rescue a trial that’s out of money.
Just as a diversified investment portfolio is more resilient, a clinical trial with multiple funding streams is better protected against any single source drying up. Different funding sources have different priorities and budget cycles; blending them can smooth out the financial flow. Moreover, some grants might cover certain aspects (e.g. a non-profit grant for patient recruitment initiatives, an NIH grant for laboratory analyses, and industry providing the study drug and associated costs). Diversification not only provides financial stability but can also mitigate bias. Ensure, however, that all contributors and their roles are fully transparent to maintain trust. Collaboration and co-funding arrangements (such as public-private partnerships) can be highly effective, as long as governance policies keep scientific independence intact.
Each funding body comes with its own rules and expectations. A best practice in grant management is to tailor your trial budget and operations to meet funder guidelines. For example, government grants might have caps on indirect costs or salary limits for investigators, whereas an industry sponsor might require specific milestones or data reports. By understanding these conditions early, you can design the trial’s financial plan to ensure compliance and avoid costly adjustments later. This might involve setting up separate accounting for grant funds, scheduling interim analyses to satisfy a funder’s go/no-go decision point, or including specific budget justifications for allowable expenses. This helps maintain confidence and can expedite approvals if you need to reallocate budget lines. In short, treating funders as partners and honoring their constraints is key to sustaining support.
Implementing strong financial management practices during the trial is as important as securing funding upfront. Utilize specialized clinical trial financial management software or tools to track expenditures in real time, generate budget vs. actual reports, and flag overruns early. Modern platforms (often integrated with Clinical Trial Management Systems) can automate invoicing, payments to sites, and financial reporting, reducing human error and improving transparency. Adopting such technology ensures that every dollar is accounted for and spent according to plan, which is reassuring to sponsors and auditors.
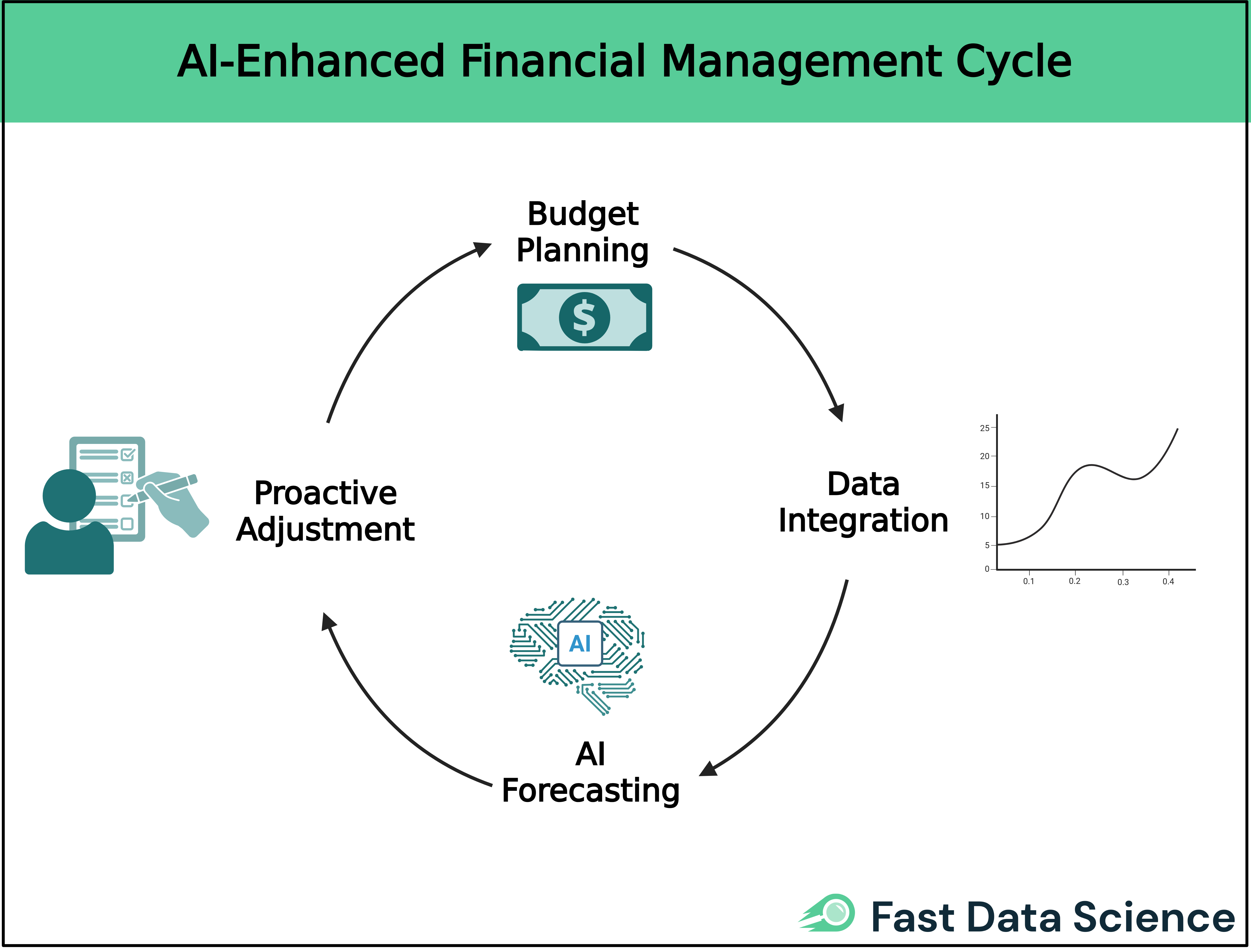
Additionally, innovative tools like AI-driven cost prediction models can be employed during trial design to forecast expenses under various scenarios [2]. For example, the Clinical Trial Risk Tool’s cost estimation module uses historical data and protocol text to predict where a trial might encounter delays or extra costs. Leveraging these insights allows teams to proactively allocate resources or adjust the trial scope before problems manifest. In practice, embracing data-driven budget management streamlines financial workflows and provides early warnings, enabling course corrections that keep the trial financially on track.
Lastly, always have a “plan B” for funding continuity. If your trial is multi-year, break the project into phases with go/no-go milestones tied to funding tranches. This way, if one phase finishes and funding isn’t immediately available for the next, you haven’t over-committed resources. Maintain relationships with secondary or backup sponsors who could step in if primary funding is lost. For example, a patient advocacy foundation might extend emergency support to bridge a gap.
Additionally, keep funders informed of the trial’s progress and significance; sometimes when cuts loom, demonstrating the real-world impact (such as patient testimonials or preliminary efficacy data) can persuade stakeholders to find ways to continue support. The unfortunate reality is that if a trial stops abruptly, “participants drift away and researchers move on to other projects that pay” [6], and the investment to date is wasted. Thus, proactive planning for continuity – financially and operationally – is a best practice that can save a trial from an untimely death.
Securing and managing clinical trial funding is challenging, but achievable with careful planning and disciplined execution. By understanding true costs, preparing for contingencies, and maintaining transparent, diversified funding, researchers can build resilient budgets that withstand uncertainty. Leveraging modern financial tools enhances efficiency and ensures every dollar serves its purpose. In an era when a single trial can cost hundreds of millions, financial stewardship is as vital as scientific integrity. Through strategic budgeting, transparency, and technology-driven management, research teams can overcome funding barriers and give promising studies the best chance to succeed, advancing medical innovation while responsibly managing the resources that make discovery possible.

Estimating the total cost of a clinical trial before it runs is challenging. Public data on past trial costs can be hard to come by, as many companies guard this information carefully. Trials in high income countries and low and middle income countries have very different costs. Upload your clinical trial protocol and create a cost benchmark with AI Protocol to cost benchmark The Clinical Trial Risk Tool uses AI and Natural Language Processing (NLP) to estimate the cost of a trial using the information contained in the clinical trial protocol.

You can download a white paper about clinical trial cost benchmarking here Estimating the total cost of a clinical trial before it runs is challenging. Public data on past trial costs can be hard to come by, as many companies guard this information carefully. Trials in high income countries and low and middle income countries have very different costs. Clinical trial costs are not normally distributed.[1] I took a dataset of just over 10,000 US-funded trials.

Guest post by Safeer Khan, Lecturer at Department of Pharmaceutical Sciences, Government College University, Lahore, Pakistan Introduction The success of clinical studies relies heavily on proper financial planning and budgeting. These processes directly impact key factors such as project timelines, resource allocation, and compliance with regulatory requirements. The accurate forecasting of costs for clinical trials, however, is a highly complex and resource-intensive process. A study by the Tufts Center for the Study of Drug Development found that the average cost of developing a new drug is approximately $2.