
The key advantage of adaptive clinical trial design is the convenience and flexibility of prospective planning opportunities to modify the study design, test hypotheses based on interim results and control or eliminate bias, which is not possible in conventional clinical trial design.
For example, based on interim data, a model-based approach could be employed to modify or optimize Phase 2 clinical trial doses based on patient’s dose-response. This approach could eliminate suboptimal dose risk and improve the drug efficacy rate without any safety signals. In the case of experimental drug inefficacy, a futility analysis can be performed without waiting for study completion to predict study failure, which drains the sponsor’s money, manpower and time. A non-adaptive trial could overestimate the treatment outcome and drug efficacy, which is technically called an under-power study and is not statistically robust.
If the estimates of variances are too conservative, there will be a risk of over-enrolment of study volunteers, subsequently leading to the wastage of resources. An adaptive clinical trial design can effectively adjust the sample size based on interim and accumulating study data and thus aids in achieving desirable clinical trial outcomes. Based on the guidelines issued by the United States Food and Drug Administration, adaptive trial designs are widely employed by clinical trial research organizations. The trial design is not arbitrary but based on rigorously-checked statistical simulation models.[1].
The Clinical Trial Risk Tool allows you to upload a protocol and will use AI and NLP to check a number of key design features in the protocol text, including adaptive design. If the protocol does not incorporate adaptive design, this is flagged to the user in a warning. You can see recommendations about the design under the section “Clinical Trial Protocol Recommendations”.
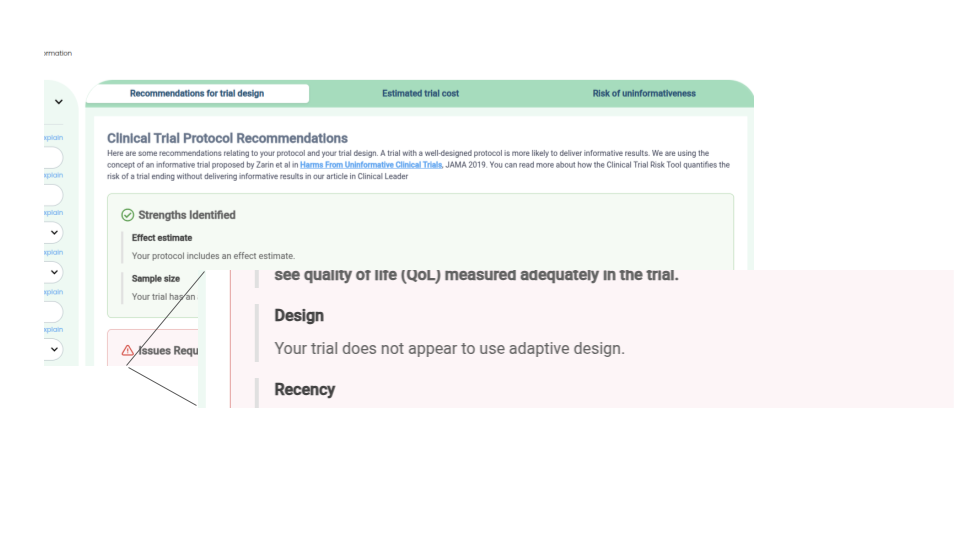
How the Clinical Trial Risk Tool displays a warning if a trial protocol does not use adaptive design
Check for adaptive design
The flexibility of adaptive clinical trial design to prospectively plan modifications in one or more aspects of the design based on outcomes (including interim data) could give an edge over non-adaptive design, in which, such planned modifications are impossible. Adaptive design involves updating a trial design based on accumulating data from subjects in that trial.
A familiar example of adaptive design exists in early-phase dose escalation studies. These studies often employ prospectively planned interim reviews of pharmacokinetic (PK) and safety data by a review committee, which then makes decisions about how to proceed. In such cases, the protocol should clearly and prospectively define committee membership and criteria for whether to stop dosing, repeat the previous dose, or proceed to a higher dose. Non-adaptive trial designs do not include such opportunities for modification.
In a non-adaptive study design, critical study parameters are planned using assumptions and best estimates. This includes parameters such as population means and event rates, variance, dose-response effect size and location, and discontinuation rates. This can work well when estimates and assumptions are accurate, but problems can arise if they are not. Non-adaptive study designs often include elements to reduce risks associated with uncertainty.
For example, if the study is meant to determine dose response, the protocol may include multiple fixed-size randomized groups to ensure that an optimal dose is captured. Such design decisions are made with the understanding that several groups will likely be treated with suboptimal doses. In this method, the study design trades efficiency in exchange for reducing the risk that the optimal dose will be missed. In contrast, with an adaptive design, you may not have to compromise efficiency to ensure that the optimal dose is captured.
Some of the important types of adaptive clinical trial design are:
This design allows study randomization alterations depending on varied probabilities in the treatment group thus increasing the chances of success.[2]
Some of the types of this design are response-adaptive randomization, treatment-adaptive randomization etc.[3, 4]
However, this design is not suitable for long-term studies due to the possibility of study extension. [2]
This design is particularly useful to predict and prematurely terminate the study in case of safety and/or efficacy issues, based on interim analysis.[5]
This model is already in use n real world medical oncology trials to detect dose-limiting toxicity.
Based on interim data, the sample size can be adjusted or modified without compromising the statistical significance. Studies with small patient populations and subgroup analyses are not suitable for this design.[6, 7]
This design allows modifications in randomization schedules depending on varied probabilities and thus increases the successful outcomes. Covariate-adaptive randomization is one of the important procedures of this design. This design is not suitable for long-term studies.
Some of the designs are drop-the-loser design and group sample size re-estimation design, in which, study subjects who received inferior therapy can be excluded [8] and premature termination of the trial with subsequent protocol modifications with additional adaptations can be done respectively.[5]
Before the initiation of the study, the clinical study investigators and biostatistics team must evaluate the feasibility of adaptive design over conventional design. The benefits of adaptive design in time and cost-cutting with convenient execution are reviewed. The reduction in bias, Type 1 error and improved statistical power with clarity on interim analysis are important for decision-making. Upon finalising the feasibility and protocol design, the team need to prepare the regulatory documents with emphasis on the adaptive design. It is very important to blind the study team before analyzing the interim data and results to avoid potential study bias and predicting early efficacy signals, particularly in subpopulations out of the whole ITT population.
The third-party vendor statistician is an independent statistician who works with the study team to determine the practical applicability of adaptive designs. This includes evaluating and comparing the benefits of adaptive design and presenting the findings to the study team. This approach could reduce or eliminate Type I errors, reduce study duration length and improve study power. The independent statistician should also communicate the findings and presentations to the data monitoring committee (IDMC) to ensure transparency and also for the smooth implementation of adaptive design.
Among all the roles of adaptive design implementation, IDMC plays a key role in ensuring patient’s right and confidentiality in a clinical trial. In addition to conventional responsibilities, IDMC is responsible for efficacy monitoring and recommending adaptations in designs such as modifications or termination of the trial.
Some of the other members of the adaptive design implementation are the sponsor executive committee comprised of biostatisticians, principal investigators and regulatory experts of the study/ They are empowered to make final decisions on the recommendations of IDMC with subsequent communication of the same with other teams. The statistical team is independent but not involved directly in the study and clinical operations. They are involved in unblinding the data and presenting the results to IDMC team. ISC communicates the workflow with IDMC to prompt the review. The latter should recommend the adaptation based on treatment efficacy and safety. Until then the study team remains blinded to the data and adaptations to eliminate bias.
The protocol is basically a guide with a description of the adaptation to signify the statistical validity. The pre-specified mandate of the protocol is to maintain the integrity of adaptive design with sample size specifications, controlling bias etc. Some of the key components are plans for statistical analysis and methodology including testing techniques such as testing the power of the study, calculations and formulas. An additional document for adaptation procedures should also be prepared to implement adaptive design.
Other important documents such as the IDMC charter and its appendix are the key to mentioning the implementation procedure of adaptive design and confidential rules, respectively.[9]
The foremost practical challenge is conducting the study with randomization and without randomization errors. In multi-arm, larger studies, the randomization may get hit due to patient discontinuation and discontinuous drug supply due to drug demand, which is usually unpredictable. Adaptive clinical trial design is armed with validated and easy-to-use statistical software for automated randomization based on patient cohorts and sample size.[10, 11, 12]
However, utilizing CRO- and indication-based personalized software is very important though the programming of software may take some time, which is one of the few practical challenges of implementing adaptive design.[13, 14]
Ensuring careful interpretation of the study results and high-quality result reporting (transparent and repeatable with highlighting of potential bias) will negate these minor inconveniences.[15, 16]
Reporting the study results and interactions with the regulatory bodies such as USFDA is a key step to amend or propose adaptive design during a study. The nature of the interaction is to ensure FDA’s review and feedback on the ongoing study as well as on the adaptive design (amendments). The type of the meeting depends on the stages of the study and the FDA’s responses are recorded in written format. The agency’s review of proposed adaptive design trial and amendments and the minutes of the closed meeting must be confidential, when the patients safety are at risk
The complexity of an adaptive design document plan is higher than non-adaptive protocol and hence submission of documents before initiating adaptive design trial is important. The confidential verification of patient selection, data monitoring and treatment randomization/assignment and locking access to these information to trial investigators etc are the few standard operating procedures of agency meeting and data review
Extensive implementation and application of adaptive trial design could aid and accelerate the drug discovery process. The adaptive design could be coupled with other novel tools including AI and complex biostatistical methods to run large clinical trials. [17, 18]
The scientific flexibility of adaptive clinical study design could be rapidly adopted across global clinical research facilities and will likely benefit the sponsors, investigators and study participants with better financial and healthcare implications.
In simpler terms, adaptive study design can be implemented in all phases of the clinical trials to achieve efficient, scientifically and statistically robust clinical trials without redundant sample size with optimized dose and patient population in confirmatory trials including RCTs. With the widespread implementation of adaptive design in clinical trials, CROs and sponsors can bring promising therapeutic drugs faster to the market. [19, 9]
Kristian T, Jonas H, Jay P, Edward JM. Key design considerations for adaptive clinical trials: The BMJ - The Research Methods & Reporting. 2018;360:k698
Shein-CC & Mark C. Adaptive design methods in clinical trials – A review. Orphanet J Rare Dis. 2008;3:11
Shein CC & Jun S. Inference of clinical trials with some protocol amendments, J Biopharm Stat. 2005;15(4):659-66
Rosenberg W, Stallard N, Ivanova A, Harper C & Ricks M. Optimal adaptive designs for binary response trials. Biometrics. 2001; 57(3):909-13
Christopher J & Bruce T, Meta-analyses and adaptive group sequential designs in the clinical development process. J Biopharm. Stat. 2005;15(4):537-58.
Liu Q & Chi G. On sample size and interference for two-stage adaptive design, Biometrics. 2001. 57(1):172-7
James H, Cui H, Wang S and Lawrence J. Adaptive statistical analysis following sample size modifications based on interim review of effect size. J Biopharm Stat. 2005; 15(4):693-706.
Mahajan R & Gupta K. Adaptive design clinical trials. Methodology, challenges, and prospect. Indian Journal of Pharmacology. 2010; 42(4):201–207
Qing L, Jianchang L & Yunzhi L. Adaptive design implementation in confirmatory trials: methods, practical considerations and case studies. Contemp. Clin Trials. 2020; 98:106096
Peter B, Frank B, Vladimir D, Franz K & Gernot W. Twenty-five years of confirmatory adaptive designs: opportunities and pitfalls. Stat Med. 2016; 10;35(3):325-47
Zhu L, Liyun L & Yao B. Group sequential methods and software applications. The American Statistician. 2012; 65(2): 127-135.
Yevgen T. A review of available software and capabilities for adaptive designs. Practical considerations for adaptive trial design and implementation. 2014; 139-155
Gina P, Nolan W, Gautier P & Frederic D. Implementation of adaptive methods in early-phase clinical trials. 2017; 36(2):215-224
Eva M, Paul G, Weili H, Lisa K, Kenneth K, Jeff M, Qi J, Marc W, Cunshan W, Katherine W, Cynthia F & Yannis J. DIA’s Adaptive design scientific working group (ADSWG): Best practices case studies for “Less well-understood” Adaptive designs. Therapeutic innovations & regulatory science. 2017; 51:77-88
Juni P, Altman D, & Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ. 2001; 323(7303):42-46.
Andrew G. Response-adaptive clinical trials: case studies in the medical literature. Pharm Stat. 2017; 16(1):64-86
Gonzalo C, John M, Christopher G, Angeles AG, Paul A, Marcus F, Antonio GO, Stuart P, Norman S, Anders S, Frans VW. Large streamlined trials in cardiovascular disease.. Eur Heart J. 2014; 35(9):544-8
Robert C. Larger simpler trials: really, it can’t be that simple! Eur H J. 2014; 35(9):549-51
Cong C, Keaven A, Devan M, Eric R & Archie T. A 2-in-1 adaptive phase 2/3 design for expedited oncology drug development. Contemp. Clin. Trials. 2018; 64: 238-242

Estimating the total cost of a clinical trial before it runs is challenging. Public data on past trial costs can be hard to come by, as many companies guard this information carefully. Trials in high income countries and low and middle income countries have very different costs. Upload your clinical trial protocol and create a cost benchmark with AI Protocol to cost benchmark The Clinical Trial Risk Tool uses AI and Natural Language Processing (NLP) to estimate the cost of a trial using the information contained in the clinical trial protocol.

You can download a white paper about clinical trial cost benchmarking here Estimating the total cost of a clinical trial before it runs is challenging. Public data on past trial costs can be hard to come by, as many companies guard this information carefully. Trials in high income countries and low and middle income countries have very different costs. Clinical trial costs are not normally distributed.[1] I took a dataset of just over 10,000 US-funded trials.

Guest post by Safeer Khan, Lecturer at Department of Pharmaceutical Sciences, Government College University, Lahore, Pakistan Introduction The success of clinical studies relies heavily on proper financial planning and budgeting. These processes directly impact key factors such as project timelines, resource allocation, and compliance with regulatory requirements. The accurate forecasting of costs for clinical trials, however, is a highly complex and resource-intensive process. A study by the Tufts Center for the Study of Drug Development found that the average cost of developing a new drug is approximately $2.