Clinical trials have long been the foundation of medical breakthroughs, but traditional methods often stumble over slow timelines, high costs, and difficulties in finding the right participants. Artificial intelligence (AI) — a technology ready to transform this landscape by making trials faster, more affordable, and smarter.
The accelerating adoption of AI in clinical trials signals a major shift in healthcare research. It is already making significant strides in transforming clinical trials. According to AI-based Clinical Trials Market Research Report 2025, the market grew from USD 7.73 billion in 2024 to USD 9.17 billion in 2025, with projections showing it will expand at a compound annual growth rate of nearly 19%, reaching USD 21.79 billion by 2030. This rapid growth highlights how AI technologies—such as machine learning and advanced data analytics—are becoming indispensable tools in clinical research.
Traditional clinical trials are lengthy and expensive. According to a report from the U.S. Department of Health and Human Services, the average time from the start of clinical testing to drug marketing stretches over 90 months. The financial burden is equally daunting, with estimates placing the cost of bringing a new drug to market anywhere between $161 million and $2 billion.
One of the biggest obstacles slowing clinical trials is recruiting the right participants and keeping them engaged throughout the study—a challenge that frequently causes delays or weakens the quality of results. At the same time, these trials generate massive and complex datasets that demand thorough and time-consuming analysis, often further stalling progress. Adding to these difficulties is the stringent regulatory environment, where navigating compliance can be slow and prone to errors, stretching the approval process even longer. Taken together, these hurdles highlight the urgent need for innovative solutions like AI integration to streamline and enhance the clinical trial process.

AI is reshaping nearly every aspect of clinical trials. From designing smarter trials to enhancing patient monitoring and data analysis, the impact of AI is both profound and far-reaching. Some of the key areas where AI is making a significant difference include:
AI plays a pivotal role in optimizing trial protocols by simulating various scenarios and predicting potential outcomes. This capability allows researchers to refine their study designs in advance, minimizing risks and enhancing the likelihood of success. The insights gained from AI based systems allow clinical trial designers to devise protocols that are both patient-friendly and scientifically robust [1]. Additionally, several AI-Based Tools leverage predictive analytics to create smarter clinical trials with reduced risks. These tools help in designing more informative trials that not only streamline the process but also deliver results more efficiently and promptly, ensuring better outcomes for researchers, sponsors, Contract research organizations (CRO), and participants. Read more about: 5 Ways AI is Transforming Clinical Trial Risk Assessment.
Among the many factors causing delays in clinical trials, patient recruitment stands out as a major challenge, accounting for approximately 37% of trial postponements [2]. AI’s data-driven capabilities offer a powerful solution by efficiently identifying potential participants who meet the trial’s specific criteria. By analyzing vast datasets such as electronic health records, genetic profiles, and demographic information, AI can rapidly and accurately pinpoint suitable candidates, accelerating the recruitment process. Beyond recruitment, AI-powered patient engagement platforms are enhancing retention by delivering personalized experiences and timely reminders, keeping participants motivated and actively involved throughout the trial.
Patient safety is paramount in clinical trials, and AI is playing an increasingly vital role in enhancing safety monitoring. By providing real-time alerts for adverse events, AI enables researchers and healthcare providers to respond swiftly, potentially preventing serious complications and improving overall patient outcomes [3].
In addition to tracking adverse events, AI can monitor patient adherence to treatment regimens, identifying any deviations or potential issues early in the process. This proactive oversight helps ensure that participants receive the intended therapies as planned, reducing the risk of adverse events caused by missed doses or incorrect usage. Together, these AI-driven capabilities create a safer, more controlled environment that benefits both patients and researchers alike.
AI is transforming the process of regulatory compliance by automating the creation and management of regulatory documents, significantly reducing manual errors and saving valuable time. This automation guarantees that reports and submissions are accurate, consistent, and delivered promptly, easing the burden on clinical teams.
Beyond document generation, AI systems continuously monitor trial processes in real time to ensure ongoing compliance with all relevant regulations and guidelines. These intelligent systems can promptly alert researchers to any potential noncompliance, allowing for swift corrective action before issues escalate. Additionally, AI’s advanced risk assessment capabilities evaluate various aspects of the trial process, identifying potential risks early and enabling proactive measures to maintain compliance throughout the study.
By streamlining documentation, enhancing monitoring, and managing risks, AI not only reduces the likelihood of delays or rejection by regulatory authorities but also allows researchers to focus more on the scientific and clinical aspects of their work. Read more about: Regulatory Compliance with AI.
AI offers a powerful solution through advanced analytics and machine learning algorithms that significantly boost the speed and accuracy of data processing in clinical trials. By efficiently sifting through vast datasets, detecting anomalies, and delivering actionable insights, AI frees clinical researchers to concentrate on strategic decisions rather than being overwhelmed by routine data management tasks [4].
Beyond simply handling data, AI’s ability to continuously learn from new inputs marks a fundamental shift from static, predetermined protocols to dynamic, adaptive trial frameworks. These advancements not only improve decision-making but also translate into substantial time and cost savings in clinical trial execution [5]. This evolving AI-driven approach is transforming how data fuels smarter, faster, and more effective clinical research.

Looking past 2025, AI’s influence in clinical trials is set to grow even more profound. One exciting frontier is the integration of emerging technologies like blockchain with AI to bolster data security and transparency. This combination could create tamper-proof trial records that inspire greater trust among regulators, researchers, and participants alike.
Simultaneously, advances in genomics and multi-omics data will empower AI to design clinical trials with unprecedented precision. By tailoring therapies to individual genetic profiles, AI will help deliver more personalized and effective treatments. Meanwhile, the Internet of Things (IoT) will connect a growing network of devices that continuously stream patient data, providing richer insights in real time.
Some experts foresee a future where clinical trials become fully autonomous. In this vision, AI systems will handle everything—from designing the trial and recruiting participants to monitoring progress, analyzing data, and generating reports—with minimal human involvement. While such fully AI-driven trials may still be a decade away, the groundwork for this transformation is being laid today.
While AI holds tremendous promise for transforming clinical trials, it also brings significant challenges that must be carefully managed. Ethical concerns surrounding bias and transparency in AI algorithms are critical issues. Without rigorous oversight, AI systems risk perpetuating unfair or inequitable outcomes, particularly in healthcare where patient diversity is vast. To address these risks, robust ethical frameworks are essential to ensure responsible AI use, a point underscored by studies examining the intersection of ethics and AI in healthcare [6, 7].
In addition to ethical concerns, regulatory complexities present substantial hurdles for AI integration. The successful adoption of AI in clinical trials demands close collaboration among stakeholders—including researchers, technology developers, and regulatory authorities—to develop clear, adaptive guidelines that keep pace with innovation while ensuring patient safety. Moreover, education and training on AI applications is also necessary for clinicians and trial staff to navigate these changes effectively [8, 9]. Balancing innovation with ethical responsibility and regulatory compliance will be key to unlocking AI’s full potential in clinical research
Roche’s “Lab in a Loop”: Genentech, a member of the Roche Group, leveraged AI and machine learning (ML) to transform drug discovery. Their innovative approach, known as the Lab in a Loop brings generative AI directly into the drug discovery and development process.
Data from laboratory experiments and clinical settings are used to train AI models and algorithms designed by Genentech’s researchers. These models then make predictions about drug targets, therapeutic molecules, and more. The predicted outcomes are tested back in the lab, generating new data that further refines and retrains the AI models to improve their accuracy. This continuous feedback loop moves beyond the traditional trial-and-error approach, accelerating the discovery of novel therapies. Read more about:
Pfizer’s AI Journey to Drug Discovery: Pfizer accelerates drug development by leveraging advanced computing techniques like modeling and simulation (M&S), which effectively bridge the gap between laboratory research and clinical application. By harnessing AI’s potential, the company rapidly developed the COVID-19 vaccine despite the historically low success rate—around 12%—for drugs advancing through clinical trials. This “bench-to-bedside” approach was also key to the successful development of neurontin (gabapentin) and remains a cornerstone of Pfizer’s innovative drug discovery pipeline today. Read more: Pfizer’s AI Journey to Drug Discovery.
AI-Powered Trial Design and Site Selection at Novartis: Novartis is leading the charge in modernizing clinical trials by integrating AI to improve AI for Trial Feasibility and Site Selection. By leveraging AI, Novartis streamlines these critical steps, enhancing efficiency and reliability, which ultimately accelerates clinical trial timelines and improves their success rates. In addition to site selection, Novartis has utilized AI-driven simulations to develop adaptive trial protocols for autoimmune diseases. These adaptive protocols allow for dynamic dose adjustments during trials, leading to faster regulatory approvals while minimizing patient risk.
AI is rapidly reshaping clinical trials by addressing long-standing challenges around cost, speed, and patient safety. It is poised to become a foundational technology—powering smarter patient recruitment, real-time monitoring, adaptive trial designs, and more precise data analysis. Yet, this progress demands a careful balance between innovation and responsible oversight. Safeguarding patient privacy, ensuring fairness in AI applications, and fostering collaboration across the healthcare ecosystem are crucial to unlocking AI’s full potential.
Meena, R.C., et al., Sustainability and reachability of healthcare through artificial intelligence. 2023.
Chaudhari, N., et al., Recruitment and retention of the participants in clinical trials: challenges and solutions. Perspectives in clinical research, 2020. 11 (2): p. 64-69.
Choudhury, A. and O. Asan, Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR medical informatics, 2020. 8 (7): p. e18599.
Ramkumar, P.N., et al., Clinical and research medical applications of artificial intelligence. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 2021. 37 (5): p. 1694-1697.
Lindsell, C.J., W.W. Stead, and K.B. Johnson, Action-informed artificial intelligence—matching the algorithm to the problem. Jama, 2020. 323 (21): p. 2141-2142.
Hammood, Z., Artificial Intelligence in Applied Medicine. Barw Medical Journal, 2023.
Hermansyah, M., et al., Artificial intelligence and ethics: Building an artificial intelligence system that ensures privacy and social justice. International Journal of Science and Society, 2023. 5 (1): p. 154-168.
Rattan, P., D.D. Penrice, and D.A. Simonetto, Artificial intelligence and machine learning: what you always wanted to know but were afraid to ask. Gastro Hep Advances, 2022. 1 (1): p. 70-78.
Sulthan, N. and S. Navas, Knowledge and attitude of artificial intelligence (AI) technology among clinical researchers in the Kingdom of Saudi Arabia. Int J Health Sci, 2022. 6 (S4): p. 5937-5947.

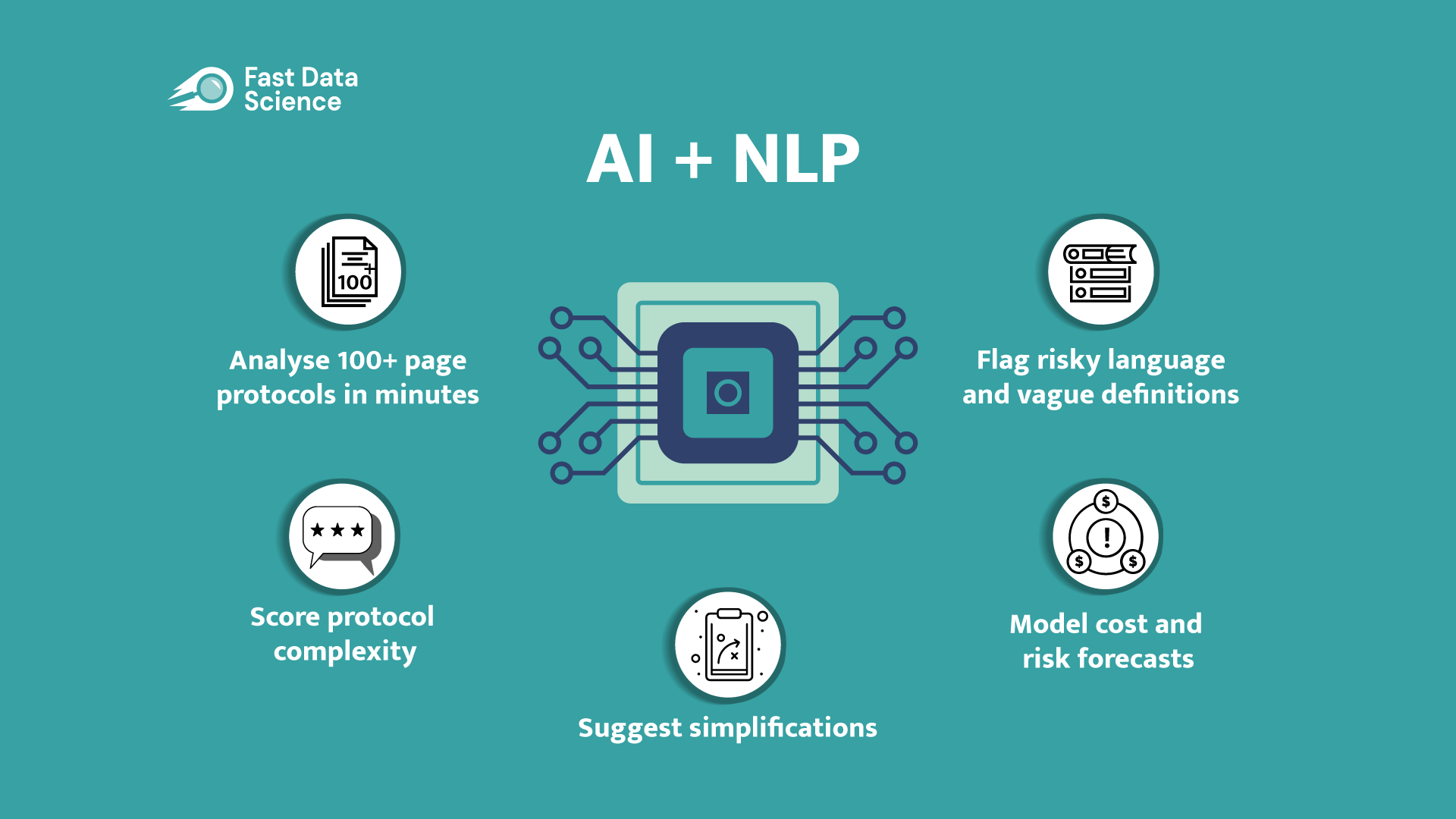
Estimating the total cost of a clinical trial before it runs is challenging. Public data on past trial costs can be hard to come by, as many companies guard this information carefully. Trials in high income countries and low and middle income countries have very different costs. Upload your clinical trial protocol and create a cost benchmark with AI Protocol to cost benchmark The Clinical Trial Risk Tool uses AI and Natural Language Processing (NLP) to estimate the cost of a trial using the information contained in the clinical trial protocol.

You can download a white paper about clinical trial cost benchmarking here Estimating the total cost of a clinical trial before it runs is challenging. Public data on past trial costs can be hard to come by, as many companies guard this information carefully. Trials in high income countries and low and middle income countries have very different costs. Clinical trial costs are not normally distributed.[1] I took a dataset of just over 10,000 US-funded trials.

Guest post by Safeer Khan, Lecturer at Department of Pharmaceutical Sciences, Government College University, Lahore, Pakistan Introduction The success of clinical studies relies heavily on proper financial planning and budgeting. These processes directly impact key factors such as project timelines, resource allocation, and compliance with regulatory requirements. The accurate forecasting of costs for clinical trials, however, is a highly complex and resource-intensive process. A study by the Tufts Center for the Study of Drug Development found that the average cost of developing a new drug is approximately $2.